Effect of Rotary Instrument Associated with Different Irrigation Techniques on Removing Calcium Hydroxide Dressing
Abstract
Calcium hydroxide [Ca(OH)2] residues in root canals may compromise sealing of filling and endodontic treatment success. The aim of this study was to compare the efficacy of using rotary instrument associated with EndoActivator, EndoVac, passive ultrasonic irrigation (PUI), and conventional needle irrigation (CNI), in Ca(OH)2 removal from root canal, by means of scanning electron microscopy (SEM) images. Sixty-six human canines were prepared with the Protaper system up to F5 and filled with Ca(OH)2. After 7 days, Ca(OH)2 was removed with rotary instrument F5 associated with the irrigation techniques used in each group (n = 15): GI (CNI), GII (EndoVac), GIII (EndoActivator) and GIV (PUI). In all groups 15 mL of 2.5% NaOCl and 3 mL of 17% EDTA were used for Ca(OH)2 removal. The Ca(OH)2 residues was evaluated by SEM in the middle and apical third using a system of scores. The results were analyzed by the Kruskal-Wallis and Dunn tests (α = 0.05). None of the techniques completely removed the Ca(OH)2 from root canals. There was no difference between EndoActivator, EndoVac and PUI (P > 0.05), but the three techniques removed more Ca(OH)2 than the CNI (P < 0,05), in the middle and apical thirds of the root canal. It was concluded that the rotary instrument combined with EndoActivator, EndoVac, and PUI was shown to be more efficient than the rotary instrument combined with the CNI in removing Ca(OH)2 from the root canal.
Introduction
Calcium Hydroxide [Ca(OH)2] has been widely used as an intracanal medication, due to its antimicrobial properties and its biological effects (Mohammadi and Dummer, 2011; Pereira et al., 2012). Nevertheless, this medication must be removed before the filling is placed, in order to obtain a better interface between the root canal walls and the filling material (Barbizam et al., 2008). Ca(OH)2 resides may diminish the bond of the cement (Barbizam et al., 2008), prevent its penetration into the dentinal tubules (Calt and Serper, 1999), increase apical leakage (Adel et al., 2012) and compromise the prognosis of endodontic treatment (Ricucci and Langeland, 1997).
The method most frequently described for removing Ca(OH)2 from the root canal is the recapitulation of the master apical file in association with irrigation with sodium hypochlorite (NaOCl) and ethylenediaminetetraacetic acid (EDTA) using conventional needle irrigation (CNI) (Lambrianidis et al., 1999; Kenee et al., 2006; Rödig et al., 2010a).
Studies have shown that the negative pressure irrigation system—EndoVac (Discus Dental, Culver City, CA), the sonic agitation system—EndoActivator (Dentsply Tulsa Dental, OK) and passive ultrasonic irrigation (PUI) are more efficient in removing Ca(OH)2 from the root canal than the CNI (Kenee et al., 2006; Wiseman et al., 2011; Yücel et al., 2011). Nevertheless, none of these methods completely remove Ca(OH)2 from the root canal, particularly from the apical third (Kenee et al., 2006; Kuga et al., 2010; Wiseman et al., 2011; Yücel et al., 2011). Furthermore, there is no consensus in the literature about which is the best technique for the removal of Ca(OH)2 (Tasdemir et al., 2011).
The rotary instrument associated with the CNI has also been recommended for removing Ca(OH)2 from the root canal (Kenee et al., 2006; Kuga et al., 2012, 2010) and has shown efficiency similar to that of PUI (Kenee et al., 2006) and better than that of the manual instrument associated with CNI. Moreover, when rotary instruments are used for Ca(OH)2 removal from the root canal, there is no difference between the various irrigant solutions used with the CNI, showing that the rotary instrument has more influence than the irrigant solution on the removal of Ca(OH)2 from the root canal (Kuga et al., 2010).
However, it is not known whether the use of the rotary instrument associated with sonic and ultrasonic agitation of the irrigant, or with the negative pressure irrigation system could increase the efficacy of Ca(OH)2 removal from the root canal. The null hypothesis tested was that the rotary instrument used in association with PUI, EndoActivator or Endovac would not increase the removal of Ca(OH)2 from the root canal, compared with the use of the rotary instrument associated with the CNI.
Materials and methods
Sixty-six freshly extracted permanent human canines stored in 1% thymol solution were obtained from the tooth bank. Teeth presenting apical curvature, root fracture, or crack, previous endodontic treatment and presence of external or internal root resorption were not included in the study.
The tooth crowns were removed 18 mm from the apex and composite resin was placed on each root tip to prevent irrigant extrusion from the apical foramen. The cervical and middle thirds of the root canals were prepared using S1 and SX instruments (ProTaper System – Dentsply Maillefer, Ballaigues, Switzerland). The working length was established as 1.0 mm short of the total tooth length. Preparation of the root canals was performed using the ProTaper Universal rotary system (Dentsply Maillefer) from S1 to F5 under irrigation with 2.5% NaOCl. After biomechanical preparation, the root canals were irrigated with 5 mL of 17% EDTA (Biodinâmica, Ibiporã, PR, Brazil), 5.0 mL of 2.5% NaOCl, dried with absorbent paper points, filled with Ca(OH)2 paste (Calen; S.S.White Artigos Denta´rios, Rio de Janeiro, RJ, Brazil) using a lentulo spiral and radiographed. The coronal access cavities were sealed with a cotton pellet and Coltosol (Coltène, WhaleDent, Switzerland). All specimens were kept in 100% relative humidity at 37◦C for 7 days and then they were randomly distributed into four groups (n = 15) according to the Ca(OH)2 removal technique: CNI (control group); EndoVac (Discus Dental); EndoActivator (Dentsply Tulsa Dental) and PUI. The specimens of the four groups were submitted to a protocol that included irrigation with 5 mL of 2.5% NaOCl, use of rotary instrument F5, irrigation with 5 mL of 2.5% NaOCl, 3 mL of 17% EDTA, and 5 mL of 2.5% NaOCl.
In all the groups the Ca(OH)2 removal technique began with irrigation with 5 mL of NaOCl, and use of rotary instrument F5. After this, in CNI group, irrigation was performed with 5 mL of NaOCl, 3 mL of EDTA and 5 mL of NaOCl. In EndoVac group irrigation was performed with 2.5 mL of NaOCl using a macrocannula, and after this, with a microcannula placed at the working length, irrigation was performed with 2.5 mL of NaOCl, 3 mL of EDTA, and 5 mL of NaOCl. In EndoActivator group and PUI group irrigation was performed in the same way as in CNI group, with each irrigant being agitated with the use of the EndoActivator or PUI for 20 s, respectively. The total activation time was 60 s. The EndoActivator was used at a frequency of 10,000 cycles/minute, with a 35.04 tip, positioned at 2 mm from the working length. For PUI a 15/.02 file was used, mounted in an ultrasonic appliance (Varios 350/350 lux, NSK, Japan) at the power of 3, positioned at 2 mm from the working length.
Except during the use of EndoVac, the irrigant solutions were placed in 5-mL syringes (Ultradent Products, South Jordan, UT) with an endodontic needle 30G (Ultradent), which was placed inside the root canal 2 mm short of the working length.
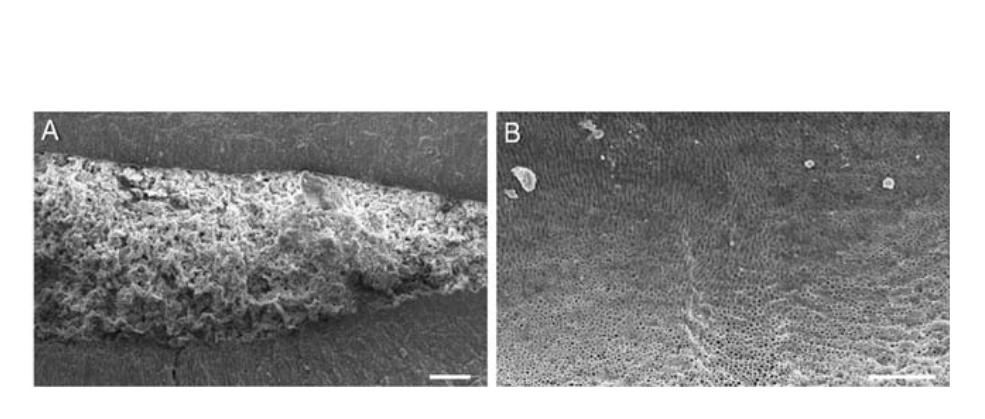
In three specimens the canal was not filled with Ca(OH)2 (negative control) and in another 3 Ca(OH)2 was not removed (positive control).
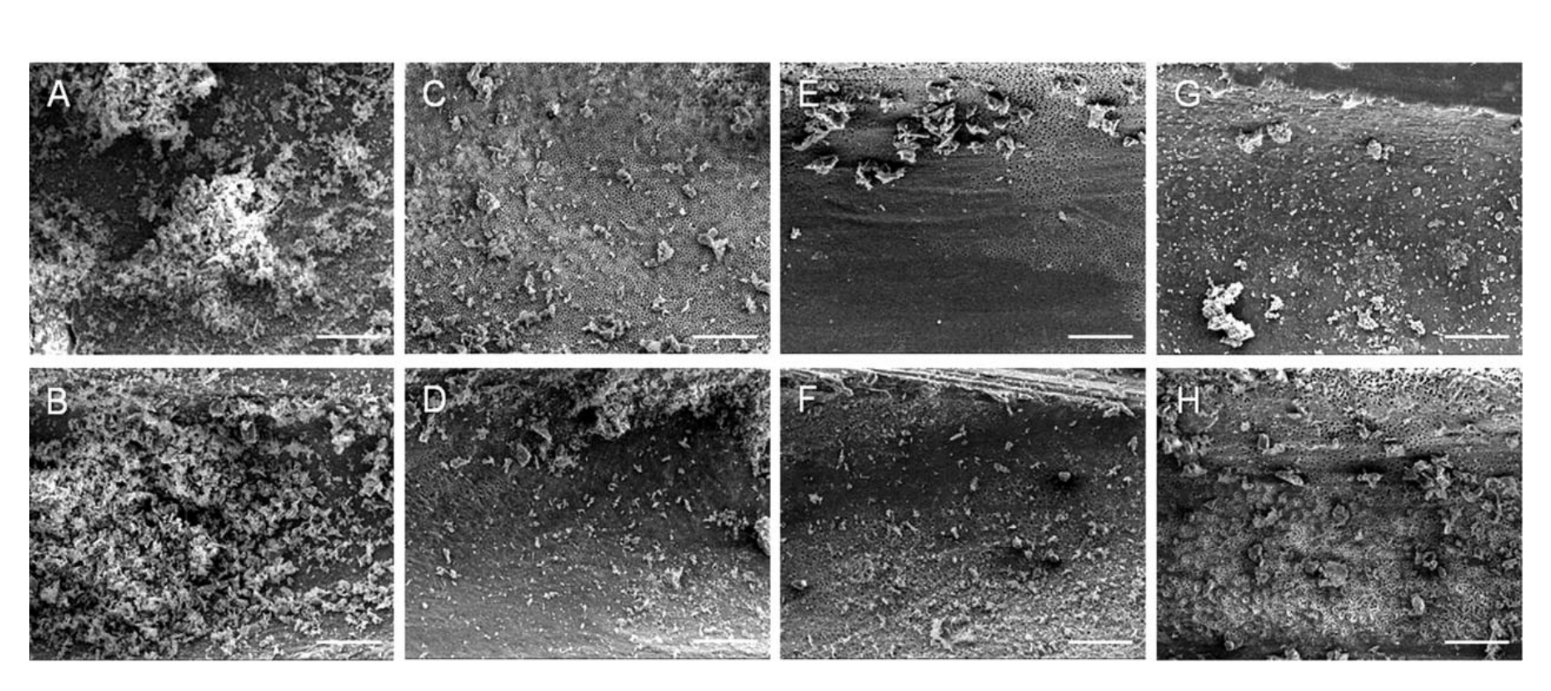
Scanning Electron Microscopy (SEM) Evaluation
The roots were split longitudinally, prepared for SEM analysis and examined under a scanning electron microscope at 20 kV (EVO 50, Carl Zeiss, Oberkochen, Germany). The residual Ca(OH)2 was visualized at 5003 magnification and two representative SEM photomicrographs were taken at 5003 magnification in the middle and apical thirds of each specimen. The amount of Ca(OH)2 debris was scored using the following system: 1, clean root canal wall, with only a few small particles of debris; 2, few small agglomerations of debris; 3, many agglomerations of debris covering less than 50% of the root canal wall; 4, more than 50% of the root canal wall covered with debris; and 5, root canal wall completely or almost completely covered with debris (Huslmann et al., 1997). Evaluation was done by two calibrated and blinded evaluators. The scores were compared, and when there was a difference, the evaluators jointly examined the sample and its scoring until they reached agreement on the score.
Statistical comparisons between groups were made by the non-parametric Kruskal-Wallis test and Dunn post-test. Comparisons between the thirds within each group were made by the Wilcoxon test (α = 0.05).
Results
None of the techniques completely removed the Ca(OH)2 from root canals. Table 1 shows the comparison between groups. There was no difference between the use of the rotary instrument combined with the EndoActivator, EndoVac and PUI (P > 0.05), and these three techniques removed significantly more Ca(OH)2 than the rotary instrument combined with the CNI (P < 0.05), both in the middle and apical thirds of the root canal. Therefore, the null hypothesis was rejected.
When comparing the efficacy of each technique with regard to the root canal third, it was verified that the EndoActivator and EndoVac removed more Ca(OH)2 in the middle third compared with the apical third of the root canal (P < 0.05). In the CNI and PUI groups, there was no difference in the Ca(OH)2 residues in the middle and apical thirds (P > 0.05). The negative controls presented no Ca(OH)2 residues on the dentinal walls, while the positive controls presented root canals completely filled with Ca(OH)2 (Fig. 1). The SEM images representative of the middle and apical thirds of the specimens in each group are shown in Figure 2.
Discussion
In this study, the efficacy of the use of a rotary instrument associated with the EndoActivator, Endo-Vac, PUI or with the CNI, in the removal of Ca(OH)2 from the root canal, was compared by means of analysis of SEM images. The use of the rotary instrument combined with the EndoActivator, EndoVac and PUI led to the removal of a larger amount of Ca(OH)2 than its use combined with the CNI.
The CNI is relatively inefficient in cleaning the apical third of the root canal (Abou-Rass and Piccnlino, 1982) because it takes the irrigant to a point no more than 1 mm short of its tip (Boutsiokis et al., 2009) and cannot be placed very close to the apical foramen, due to the increased chances of extrusion of the solution (Druttman and Stock, 1989). The EndoVac, a negative pressure aspiration/irrigation system was developed with the purpose of irrigating and removing debris from the apical third of the root canal safely, without forcing irrigants into the periapical tissues (Nielsen and Baumgartner, 2007; Shin et al., 2010; Munoz and Camacho-Cuadra, 2012). This system consists of a macrocannula and a microcannula that are connected to a high speed suction device (Nielsen and Baumgartner, 2007). It creates a negative pressure system that pulls the irrigant from the pulp chamber into the root canal and evacuates the irrigant solution and the debris by means of small orifices in the cannula coupled to the suction device (Nielsen and Baumgartner, 2007; Gu et al., 2009; Shin et al., 2010). Studies have shown that the EndoVac is more efficient in taking the irrigant to the working length (Munoz and Camacho-Cuadra, 2012) and in removal of the debris and smear layer from the apical third of the root canal, in comparison with the CNI (Nielsen and Baumgartner, 2007; Shin et al., 2010).
In this study, the EndoVac system was more efficient in removing Ca(OH)2 from the root canal than the CNI, and showed no difference from the EndoActivator and PUI. These results are in agreement with those of previous studies in straight or curved root canals, which showed that irrigation with EndoVac improved Ca(OH)2 removal, resulting in cleaner root canals than those obtained with the use of CNI (Yu€cel et al., 2011; Goode et al., 2013). They are also in agreement with the results of a study that found no difference between the efficacy of EndoVac and PUI in the removal of Ca(OH)2 (Yücel et al., 2011). Goode et al. (2013) showed that the EndoVac removed significantly more Ca(OH)2 from the sulcus made in the apical third in models of curved canals, when compared with the CNI, EndoActivator, continuous ultrasonic irrigation, manual agitation with a gutta-percha cone and with the negative pressure irrigation system - VPro EndoSafe.
The EndoActivator, a sonically activated device, produces vigorous agitation of the irrigant by activation of a tip composed of a flexible, non-cutting polymer (Ruddle, 2007; Desai and Himel, 2009; Gu et al., 2009) with the purpose of increasing the removal of debris and smear layer (Ruddle, 2007). The EndoActivator presents greater efficiency in debris removal than the PUI and CNI (Kanter et al., 2011) and is more efficient in smear layer removal than the CNI (Blank-Gonçalves et al., 2011). In this study, the use of the EndoActivator in combination with the rotary instrument results in significantly cleaner canals, when compared with the use of the rotary instrument associated with the CNI, but it was not better than the PUI and EndoVac.
In PUI a thin smooth tip is introduced into the canal filled with irrigant solutions and is activated by means of ultrasound; so that acoustic microstreaming occurs around the instrument (Van der Sluis et al., 2007), producing agitation of the irrigant solution (Gu et al., 2009). This agitation creates intense movement of the irrigant around the instrument, with a flow directed towards the apical region (Desai and Himel, 2009). Thus the irrigant solution is more easily able to penetrate into the irregularities of the root canal system (Van der Sluis et al, .2007) and into the working length (Munoz and Camacho-Cuadra, 2012), providing better cleaning than the CNI (Van der Sluis et al., 2007; Jiang et al., 2011). Various studies have shown that the NaOCl solution associated with PUI, in the final stage of irrigation removes more debris, bacteria and pulp tissue when compared with the CNI (Van der Sluis et al., 2007; Al-Jadaa et al., 2009; Rödig et al., 2010b; Jiang et al., 2011).
According to the literature, in single rooted teeth, the PUI was shown to be more effective than the CNI for the removal of Ca(OH)2 (Kenee et al., 2006; Van der Sluis et al., 2007; Tasdemir et al., 2011). In root canals of the mesial root of mandibular molars, Wiseman et al. (2011) verified that the PUI was more efficient than the EndoActivator for the removal of Ca(OH)2. Whereas, Khaleel et al. (2013) found no difference between the EndoActivator and PUI, as both were more effective in the removal of Ca(OH)2, than the CNI single rooted teeth.
Comparing the thirds of the same groups, the Endo-Vac and EndoAtivator removed more Ca(OH)2 in the middle third compared with the apical third of the root canal which is in accordance with investigations that showed more Ca(OH)2 residues in the apical thirds of the root canal after the use of these appliances (Yücel et al., 2011; Khaleel et al., 2013). However, in the CNI and PUI groups, there was no difference in the Ca(OH)2 residues in the middle and apical thirds, which is in contrast to other investigations that found Ca(OH)2 residues mainly in the apical region after use of CNI or PUI (Yücel et al., 2011; Khaleel et al., 2013). On the other hand, some studies have been found no significant difference between the thirds of the canal in groups where CNI (Salgado et al., 2009) or CNI plus patency (Lambrianidis et al., 2006) were used for Ca(OH)2 removal. Other study showed that Ca(OH)2 removal using CNI was superior in the root apical third compared with the coronal third (Rödig et al., 2010a).
The results of this study showed that the rotary instrument associated with the CNI was not sufficient to remove the Ca(OH)2 from the root canal. The use of the rotary instrument associated with the EndoVac, EndoActivator, and PUI improved the removal of Ca(OH)2 resulting in cleaner root canals. Nevertheless, none of the techniques completely removed the Ca(OH)2 from the root canal, and this is in agreement with previous studies that found residues of this medication in the root canal, irrespective of the use of different irrigation/agitation systems of irrigants and devices, such as laser, for example (Van der Sluis et al., 2007; Kuga et al., 2010; Silva et al., 2011; Tasdemir et al., 2011; Wiseman et al., 2011; Kaptan et al., 2012; Goode et al., 2013). Thus, future researches must be conducted, using other techniques for Ca(OH)2 removal from the root canal.
It was concluded that the rotary instrument combined with EndoActivator, EndoVac and PUI was more efficient than the rotary instrument combined with the CNI in removing Ca(OH)2 from the root canal.
Gisele Faria, Kennia Scapin Viola, Milton Carlos Kuga, Arturo Javier Aranda Garcia, Vanessa Bossolani Daher, Mário Francisco De Pasquali Leonardo, Mário Tanomaru-Filho
References
- Abou-Rass M, Piccinino MV. 1982. The effectiveness of four clinical irrigation methods on the removal of root canal debris. Oral Surg Oral Med Oral Pathol 54:323–328.
- Adel M, Foroozia M, Rezaei MH, Mahboobi N. 2012. Effect of calcium hydroxide on the apical leakage of Resilon-filled root canals: An in vitro study. Gen Dent 60:136–140.
- Al-Jadaa A, Paqué F, Attin T, Zehnder M. 2009. Acoustic hypochlorite activation in simulated curved canals. J Endod 35:1408–1411.
- Barbizam JV, Trope M, Teixeira EC, Tanomaru-Filho M, Teixeira FB. 2008. Effect of calcium hydroxide dressing on the bond strength of a resin-based endodontic sealer. Braz Dent J 19:224–227.
- Blank-Gonçalves LM, Nabeshima CK, Martins GH, Machado ME. 2011. Qualitative analysis of the removal of the smear layer in the apical third of curved roots: Conventional irrigation versus activation systems. J Endod 37:1268–1271.
- Boutsiokis C, Lambrianidis T, Kastrinakis E. 2009. Irrigant flow within a prepared root canal using various flow rates: A computational fluid dynamics study. Int Endod J 42:144–155.
- Calt S, Serper A. 1999. Dentinal tubule penetration of root canal sealers after root canal dressing with calcium hydroxide. J Endod 25: 431–433.
- Desai P, Himel V. 2009. Comparative safety of various intracanal irrigation systems. J Endod 35:545–549.
- Druttman AC, Stock CJ. 1989. An in vitro comparison of ultrasonic and conventional methods of irrigant replacement. Int Endod J 22: 174–178.
- Goode N, Khan S, Eid AA, Niu LN, Gosier J, Susin LF, Pashley DH, Tay FR. 2013. Wall shear stress effects of different endodontic irrigation techniques and systems. J Dent 41:636–641.
- Gu LS, Kim JR, Ling J, Choi KK, Pashley DH, Tay FR. 2009. Review of contemporary irrigant agitation techniques and devices. J Endod 35:791–804.
- Hulsmann M, Rummelin C, Schafers F. 1997. Root canal cleanliness after preparation with different endodontic handpieces and hand instruments: A comparative SEM investigation. J Endod 23:301– 306.
- Jiang LM, Verhaagen B, Versluis M, Langedijk J, Wesselink P, van der Sluis LW. 2011. The influence of the ultrasonic intensity on the cleaning efficacy of passive ultrasonic irrigation. J Endod 37:688– 692.
- Kanter V, Weldon E, Nair U, Varella C, Kanter K, Anusavice K, Pileggi R. 2011. A quantitative and qualitative analysis of ultrasonic versus sonic endodontic systems on canal cleanliness and obturation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112:809–813.
- Kaptan F, Karapinar-Kazandag M, Kayahan MB, Bora T, Bayirli G. 2012. Potential of an Er:YAG laser in the removal of calcium hydroxide from root canals. Photomed Laser Surg 30:250–254.
- Kenee DM, Allemang JD, Johnson JD, Hellstein J, Nichol BK. 2006. A quantitative assessment of efficacy of various calcium hydroxide removal techniques. J Endod 32:563–565.
- Khaleel HY, Al-Ashaw AJ, Yang Y, Pang AH, Ma JZ. 2013. Quantitative comparison of calcium hydroxide removal by EndoActivator, ultrasonic and ProTaper file agitation techniques: An in vitro study. J Huazhong Univ Sci Technolog Med Sci 33:142–145.
- Kuga MC, Campos EA, Faria-Junior NB, Só MV, Shinohara AL. 2012. Efficacy of NiTi rotary instruments in removing calcium hydroxide dressing residues from root canal walls. Braz Oral Res 26:19–23.
- Kuga MC, Tanomaru-Filho M, Faria G, S´o MV, Galletti T, Bavello JR. 2010. Calcium hydroxide intracanal dressing removal with different rotary instruments and irrigating solutions: A scanning elec- tron microscopy study. Braz Dent J 21:310–314.
- Lambrianidis T, Margelos J, Beltes P. 1999. Removal efficiency of calcium hydroxide dressing from the root canal. J Endod 25:85–88.
- Mohammadi Z, Dummer PM. 2011. Properties and applications of calcium hydroxide in endodontics and dental traumatology. Int Endod J 44:697–730.
- Munoz HR, Camacho-Cuadra K. 2012. In vivo efficacy of three different endodontic irrigation systems for irrigant delivery to working length of mesial canals of mandibular molars. J Endod 38:445–448.
- Nielsen BA, Baumgartner JC. 2007. Comparison of the EndoVac system to needle irrigation of root canals. J Endod 33:611–615.
- Pereira MS, Faria G, Bezerra da Silva LA, Tanomaru-Filho M, Kuga MC, Rossi MA. 2012. Response of mice connective tissue to intracanal dressings containing chlorhexidine. Microsc Res Tech 75:1653–1658.
- Ricucci D, Langeland K. 1997. Incomplete calcium hydroxide removal from the root canal: a case report. Int Endod J 30:418–421.
- Rödig T, Döllmann S, Konietschke F, Drebenstedt S, Hülsmann M. 2010b. Effectiveness of different irrigant agitation techniques on debris and smear layer removal in curved root canals: A scanning electron microscopy study. J Endod 36:1983–1987.
- R€odig T, Vogel S, Zapf A, Hu€lsmann M. 2010a. Efficacy of different irrigants in the removal of calcium hydroxide from root canals. Int Endod J 43:519–527.
- Ruddle CJ. 2007.Hydrodynamic disinfection: Tsunami endodontics. Dent Today 26:4–7.
- Salgado RJ, Moura-Netto C, Yamazaki AK, Cardoso LN, de Moura AA, Prokopowitsch I. 2009. Comparison of different irrigants on calcium hydroxide medication removal: Microscopic cleanliness evaluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107:580–584.
- Shin SJ, Kim HK, Jung IY, Lee CY, Lee SJ, Kim E. 2010. Comparison of the cleaning efficacy of a new apical negative pressure irrigating system with conventional irrigation needles in the root canals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:479–484.
- Silva JM, Silveira A, Santos E, Prado L, Pessoa OF. 2011. Efficacy of sodium hypochlorite, ethylenediaminetetraacetic acid, citric acid and phosphoric acid in calcium hydroxide removal from the root canal: A microscopic cleanliness evaluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112:820–824.
- Taşdemir T, Celik D, Er K, Yildirim T, Ceyhanli KT, Yeşilyurt C. 2011. Efficacy of several techniques for the removal of calcium hydroxide medicament from root canals. Int Endod J 44:505–509.
- Van der Sluis LW, Wu MK, Wesselink PR. 2007. The evaluation of removal of calcium hydroxide paste from an artificial standardized groove in the apical root canal using different irrigation methodologies. Int Endod J 40:52–57.
- Wiseman A, Cox TC, Paranjpe A, Flake NM, Cohenca N, Johnson JD. 2011. Efficacy of sonic and ultrasonic activation for removal of calcium hydroxide from mesial canals of mandibular molars: A micro-tomographic study. J Endod 37:235–238.
- Yücel A C, Gürel M, Güler E, Karabucak B. 2011. Comparison of final irrigation techniques in removal of calcium hydroxide. Aust Endod J DOI:10.1111/j.1747–44.

/social-network-service/media/default/102339/cc73e2fd.png)