Factors for Success in Tooth Autotransplantation
Traducción automática
El artículo original está escrito en idioma RU (enlace para leerlo) .
Introduction
Over the past 20 years, progress in understanding the processes of regeneration after autotransplantation and replantation has significantly impacted the success of these procedures. However, it is still not reasonable to expect the same level of success from autotransplantation as with implantation, but knowledge of healing processes allows for informed choices in certain clinical cases. Modern research has proven the possibility of restoring the periodontal ligament, thereby ensuring the success of this operation.
Mechanisms of Periodontal Ligament Healing
The fastest recovery of the periodontal ligament occurs when a tooth is transplanted back into its own socket within a short period (replantation). This type of healing is described as "reattachment" and is defined as "the union of connective tissue fibers that were separated by incision or injury." In autotransplantation, the periodontal ligament is usually torn in the middle, such that part of it remains on the root surface and part on the socket surface. The "restoration" of the periodontium in this case is due to the formation of a fibrous connection between the parts of these fibers.
Several studies have shown that this type of healing is possible with tooth transplantation only with a sufficient volume of periodontal ligament within a strictly defined time frame.
The healing process is as follows (considered according to the study by Ichinokawa H):
- on the 3rd day after replantation: clusters of fibrin and erythrocytes are found between the root's periodontal ligament and the socket.
- after 1-2 weeks: fibroblasts and collagen fibers are visible in the torn area, indicating the beginning of ligament restoration.
- after 3-4 weeks: proliferation of fibroblasts and regularly aligned bundles of collagen fibers are observed, indicating the continuation of functional restoration of the ligament.
- after 8 weeks: nearly normal periodontal ligament and evenly arranged bundles of collagen fibers are found. The time intervals may vary from one study to another, but there is a consensus that after autotransplantation and replantation, the restoration of periodontal fibers occurs. Complete healing takes about 2 months (the stage of functional alignment of fibers), but in the area of the gum and the cervical part of the root, attachment occurs within 1-3 weeks.
The restoration of the periodontal ligament during transplantation into an artificially created socket differs from the process observed when transplanting into natural sockets. The difference is due to the absence of periodontal fibers on the surface of the socket.
Healing in this type of surgery occurs differently:
- within 1 week: the periodontal fibers on the root surface remain vital due to the surrounding blood clot.
- after 2 weeks: the blood clot is replaced by granulation tissue, which also provides favorable conditions for the nutrition of ligament cells and is the initial stage of connective tissue formation.
- after 2-6 months: granulation tissue and immature bone tissue are replaced by mature bone tissue, and the tooth-alveolar connection is formed.
According to research data , there is a significantly lower number of functional periodontal fibers observed when transplanting into an artificial socket, which has been repeatedly proven histologically. In the Shimada study , it was shown that the width of the forming periodontal space is smaller. Nevertheless, clinically satisfactory healing is observed (i.e., absence of root resorption, preservation of the periodontal ligament space on X-ray, normal tooth mobility).
A comparative study conducted by Andreasen demonstrates that the prognosis of autotransplantation largely depends on the condition of the periodontal ligament on the root surface, rather than its presence in the recipient area. Defects and absence of periodontal fibers on the root surface are factors that lead to resorption. In cases of minor deficiency of periodontal fibers, recovery is possible through the regeneration of cement and the formation of new attachment. The mechanism of forming a new connection between the exposed root surface and the surrounding tissue occurs through the proliferation of root cement cells from the periphery of the defect and the embedding of Sharpey's fibers into the newly formed cement. The size of these defects and the distance to the walls of the recipient socket affect the subsequent healing outcome. The greater the distance between the root and the socket wall, the more time is needed for the bone tissue to reach the root, allowing cement cells to proliferate and close the defect area. According to Andreasen, lesions up to 2 mm in width can close without consequences for the root.
Complications and their causes. Mechanisms of root resorption
Root resorption occurs with complete or partial damage to the surface of the donor tooth root. Resorption during autotransplantation or replantation is divided into 3 types: replacement resorption, inflammatory resorption, and surface resorption. It has been proven that the type of resorption is determined by the degree of damage to the root surface and pulp infection.
Replacement resorption
Replacement resorption is the process by which the root of the tooth is resorbed and replaced by bone tissue, leading to ankylosis, the fusion of the root and bone together.
A study conducted by Ishinokawa7 on monkeys (replantation of teeth with mechanically removed periodontal ligament) demonstrated the replacement of bone tissue on the root surface within 1 week after replantation. An interesting finding in this study was that the production of bone tissue by osteoblasts from the periodontal ligament on the surface of the alveolus preceded root resorption. Furthermore, after 4 weeks, there was partial fusion of the newly formed bone on the root surface and the alveolar bone, indicating the onset of the ankylosis process in this area. Clinically, ankylosis was noted only in the fourth month after replantation. In most cases, partial ankylosis is difficult to diagnose, as the teeth retain normal mobility and also give a normal response to percussion tests. Long-term radiological observations are the only way to determine whether partial ankylosis progresses to complete root replacement or whether the root surface is restored through the formation of new cementum.
A characteristic feature of replacement resorption is that its rate depends on the age of the patient. The rate of replacement resorption is proportional to the rate of bone remodeling in the patient - up to 50% per year in children, about 2% per year in adults. This indicates that even in the event of ankylosis after transplantation in adults, the tooth can function normally for a long period of time.
Clinical case
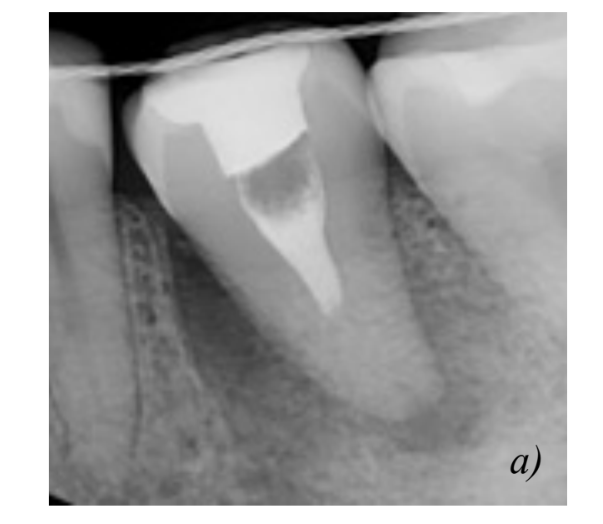
A 30-year-old female patient presented with a request to restore the missing 4.6 tooth for more than 8 years. Autotransplantation of the 2.8 tooth was performed into an artificially created alveolus using a stereolithographic model. Two weeks after the surgery, endodontic treatment of the tooth was carried out. Four weeks after the surgery, the fixing splint was removed, and the absence of pathological mobility of the tooth was recorded. Within a month, prosthetic restoration with an artificial crown was performed. Follow-up examinations were conducted at 3, 6, 12, and 18 months. During the first year, no pathological inflammatory processes or clinical signs of resorption were detected. Upon examination after 1.5 years, signs of replacement resorption were found.

The transplant is fixed with a bilateral splint, out of
occlusion.



Inflammatory Resorption
Inflammatory resorption is observed during tooth transplantation with pulpal infection and partial loss of the periodontal ligament. Bacteria and their metabolic products migrate through the canals to the root surface, causing an inflammatory response in the surrounding tissues.
The characteristic feature of inflammatory resorption is the presence of granulation tissue, which contains a large number of capillary vessels in the resorptive lacuna, making this area radiolucent. Clinically, radiolucency is observed on radiographs 1 and 2 months after transplantation. Sometimes, delayed inflammatory resorption is observed in the cervical part of the root several years after transplantation. The age of patients does not affect the rate of inflammatory resorption, which in most cases proceeds rapidly. Unlike replacement resorption, inflammatory resorption can be halted by timely endodontic treatment.
Surface Resorption
This type of resorption is limited to the layer of cement on the root surface. Surface resorption is part of the reparative mechanism, where new cement covers the resorbed areas, and the fibers of the periodontal ligament are embedded in the newly formed cement.
Surface resorption is the result of limited partial trauma to the periodontal ligament and is temporary in nature.
Clinical Case
A 29-year-old female patient presented with pain in the area of tooth 3.6. Upon examination, a fracture of the root of tooth 3.6 and chronic apical periodontitis were identified. Tooth 3.6 was extracted with simultaneous autotransplantation of tooth 3.8. Prior to this, tooth 3.8 was depulped and the root canals were filled with a calcium hydroxide-based material. Splinting was performed with a unilateral splint for 4 weeks, and the tooth was taken out of occlusion. Endodontic treatment was completed after 2 weeks. After 6 months, the crown of the tooth was restored with an artificial crown.


Prognostic Factors
The first and most important prognostic factor for the success of autotransplantation is the selection of the clinical case. The main indicator is the risk-benefit ratio, which is more favorable than for any other treatment, as well as when the tooth needs to be preserved for aesthetic and functional reasons. Suitable patients for treatment are motivated young individuals for whom dental implantation is undesirable or contraindicated. The most common clinical situations for transplantation are:
- the use of the third molar to replace the absence of the first or second molar,
- the use of an extracted premolar for orthodontic reasons to replace a central incisor,
- the repositioning of a retained canine into the correct position.
To perform the operation, it is important to obtain a complete, thoroughly collected medical history, detailed radiographic examination, measure the donor tooth and the recipient site, as well as determine the shape of the root. A contraindication for the operation may be insufficient bone volume in the recipient area, as well as the possibility of complicated extraction of the retained tooth. Compromised teeth with periodontal disease, where there has been a loss of epithelial attachment of more than 1/3, are also not suitable donors due to a lack of periodontal ligament. According to the literature, the best prognosis is observed in young patients with undeveloped apices of donor teeth. Long-term studies ranging from 3 to 14 years show that in such teeth, pulp vitality is preserved in 90-96% of cases. However, it has also been shown that tooth transplantation works at any age. The likelihood of success depends on the surgical technique, the experience and capabilities of the surgeon, as well as factors such as the age of the patient, the degree of root development, the type of transplanted tooth, time in a dry environment, positioning of the tooth, and the condition of the soft tissues of the recipient site.
Surgical technique should be as atraumatic as possible, and manipulations with the donor tooth should be minimized to preserve the periodontal ligament as well as the epithelial sheath of Hertwig, in order not to disrupt root development, avoid ankylosis, root resorption, and loss of epithelial attachment.
The transplanted tooth, after being placed in the socket, can be fixed with a cross suture over the crown or with a non-rigid splint. It has been proven that prolonged rigid splinting of the transplanted tooth has an adverse effect on periodontal healing. Thus, immobilization should be relative for a period of 2 weeks to 2 months depending on the placement of the donor tooth in the alveolus. The ideal alveolus should have sufficient width and height to fully accommodate the donor tooth. Moreover, the smaller the distance between the tooth root and the alveolar wall, the faster the rehabilitation process will occur.
In the case of transplanting third molars into the adjacent alveolus of second molars, the prognosis is worse when the wisdom tooth is significantly lower than the socket of the second molar, which may contribute to the disruption of epithelial attachment in the distal area after transplantation.
The donor tooth should be placed in the socket freely, without pressure, and it should be slightly out of occlusion during the healing period. This handling of the root ensures its further growth (in the case of underdeveloped roots) and the absence of resorptive processes.
Studies have shown that underdeveloped roots have a low success rate, and the earlier the stage of development of the transplanted tooth's roots, the less growth they provide subsequently. Thus, it has been proven that the ideal stage for transplantation is when the root is 3/4 of its length and the apical foramen is open by more than 1 mm.
In most cases, complete recovery of the periodontium is achieved within 2 months after the operation and is characterized by the absence of root resorption and the presence of a compact bone tissue plate on the X-ray. In addition, the X-ray shows a uniform space of the periodontal ligament throughout the root. Teeth with an undeveloped apex most often do not require endodontic treatment, complete the development of their roots, and maintain pulp vitality. Revascularization usually occurs 4 days after transplantation and progresses at a rate of 0.1 mm per day. It is recommended that the extraoral time of the donor tooth should not exceed 5-7 minutes; however, no direct correlation has been established between this factor and root resorption.
The treatment plan should be based on a careful selection of the clinical case in order to choose the most appropriate time for autotransplantation. For example, if a tooth in the recipient area needs to be removed urgently, then the transplantation may be postponed for no more than 2-4 weeks after extraction to preserve the socket parameters. Whenever possible, transplantation is best performed immediately after tooth extraction. If there is a predictable need for endodontic treatment, it can be done before the surgery or outside the oral cavity. If such an opportunity is not available, then endodontic treatment must be performed within 2 weeks after the surgery.
Authors: Badalyan K.Yu., Zedgenidze A.M.
References
- Kalkwarf KI. Periodontal new attachment without the placement of osseous potentiating grafts. Periodontal Abstracts 1974;2:53-62.
- American Academy of Periodontology: Glossary of Periodontal Terms J Periodontol Nov, 1986
- Löe H, Waerhaug J. Experimental replantation of teeth in dogs and monkeys. Arch Oral Biol 1961;3:176-184
- Andreasen JO. A time-related study of periodontal healing and root resorption activity after replantation of mature permanent incisors in monkeys. Swed Dent J 1980;4:101-110.
- Tobe O. Histological studies on periodontal tissue reactions following intentional replantation of incisors in monkeys: With special reference to computer-aided three dimensional reconstruction of replanted teeth [in Japanese]. Jpn J Conserv Dent 1990;33:772-802.
- Fukuro K. Bone morphometrical studies of intentional replantation in monkeys' teeth [in Japanese]. Jpn J Conserv Dent 1991; 34:957-985
- Ichinokawa H. Ultrastructural studies on periodontal tissue reactions following intentional tooth replantation in adult monkeys [in Japanese]. Jpn J Conserv Dent 1995;38:63-87.
- Proye MP, Polson AM. Repair in different zones of the periodontium after tooth reimplantation. J Periodontol 1982;53:379-389
- Ichinokawa H, et al. The pathological analysis in the experiments on autotransplantation of teeth [in Japanese]. Jpn J Conserv Dent 1998:41:38.
- Ichinokawa H, et al. The pathological analysis in the experiments on autotransplantation of teeth: Part 2. The microstructural changes in the healing process [in Japanese]. Jpn J Conserv Dent 1998;41:91
- Kurisaki H. The pathological analysis in the experiments on autotransplantation of teeth: Part 2 [in Japanese]. J Jpn Soc Oral Implantol 1998;11:270-271
- Ichinokawa H, et al. The pathological analysis in the experiments on autotransplantation of teeth: Part 4. The microstructural changes in the healing process [in Japanese]. J Jpn Soc Oral Implantol 1999;12:131
- Asai Y, Nakagawa K. PDL preservation in transplantation and replantation of teeth. Part 1. The experimental and clinical approach [in Japanese]. J Jpn Dent Assoc 1997;50:6-16.
- Shimada T. Effect of periodontal ligament curetted in alveolar socket for autotransplantation of tooth in adult monkeys [in Japanese]. J Jpn Soc Oral Implantol 1998;11:492-500
- Andreasen JO. Periodontal healing after replantation and autotransplantation of incisors in monkeys. Int J Oral Surg 1981;10 54-61
- Isono T. Effect of storage media upon periodontal healing after replantation of teeth in adult monkeys [in Japanese]. J Jpn Soc Oral Implantol 1998;11:375-385. 17.Andreasen JO. Relationship between cell damage in the periodontal ligament after replantation and subsequent development of root resorption. Acta Odontol Scand 1981;39:15-25
- Yoshida M. An experimental study on regeneration of cementum, periodontal ligament and alveolar bone in the intradentinal cavities in dogs [in Japanese]. The Shikwa Gakuho 1976;76: 1179-1222.
- Andreasen JO, Kristerson L. The effect of limited drying or removal of the periodontal ligament. Periodontal healing after replantation of mature incisors in monkeys. Acta Odontol Scand 1981;39:1-13
- Andreasen JO, Hjørting-Hansen E. Replantation of teeth. I Radiographic and clinical study of 110 human teeth replanted after accidental loss. Acta Odontol Scand 1966;24:263-286
- Andreasen JO, Hjørting-Hansen E. Replantation of teeth. II Histological study of 22 replanted anterior teeth in humans Acta Odontol Scand 1966;24:287-306
- Andersson L., Jonsson BG, Hammarström L Blomlöf L, Andreasen JO, Lindskog S. Evaluation of statistics and desirable experimental design of a histomorphometrical method for studies of root resorption. Endod Dent Traumatol 1987;3:288-295
- Andreasen JO. Experimental dental traumatology: development of a model for external root resorption. Endod Dent Traumatol 1987;3:269-287.
- Andreasen JO. Relationship between surface and inflammatory resorption and changes in the pulp after replantation of permanent incisors in monkeys. J Endod 1981;7:294-301.
- Andersson L, Bodin I, Sorensen S. Progression of root resorption following replantation of human teeth after extended extraoral storage. Endod Dent Traumatol 1989;5:38-47 45.
- Frost HM. Tetracycline-based histological analysis of bone remodeling. Calcif Tissue Res 1969;3:221-237
- Andreasen JO. External root resorption: its implication in dental traumatology, periodontics, orthodontics and endodontics. Int Endod J 1985;18:109-118
- Andreasen JO. The effect of pulp extirpation or root canal treatment on periodontal healing after replantation of permanent incisors in monkeys. J Endod 1981;7:245-252, 1982:8:426-427.
- Andreasen JO, Paulsen HU, Yu Z, Ahlquist R, Bayer T, Schwartz O. A long term study of 370 autotransplanted premolars. Part I. Surgical procedure and standardized techniques for monitoring healing. Eur J Orthod 1990;12:3-13.
- Andreasen JO, Paulsen HU, Yu Z, Bayer T, Schwartz O. A long term study of 370 autotransplanted premolars. Part II. Tooth survival and pulp healing subsequent to transplantation. Eur J Orthod 1990;12:14-24
- Andreasen JO, Paulsen HU, Yu Z, Schwartz O. A long term study of 370 autotransplanted premolars. Part III. Periodontal healing subsequent to transplantation. Eur J Orthod 1990;12:25-37.
- Andreasen JO, Paulsen HU, Yu Z, Bayer T. A long term study of 370 autotransplanted premolars. Part IV. Root development subsequent to transplantation. Eur J Orthod 1990;12:38-50
- 33.Andreasen JO. Atlas of Replantation and Transplantation of Teeth. Philadelphia: Saunders, 1992
- Andreasen JO. Analysis of topography of surface and inflammatory root resorption after replantation of mature permanent incisors in monkeys. Swed Dent J 1980;4:135-144
- Josefsson E1, Brattström V, Tegsjö U, Valerius-Olsson H. Treatment of lower second premolar agenesis by autotransplantation: four-year evaluation of eighty patients. Acta Odontol Scand. 1999 Apr;57(2):111-5.
- Kallu R1, Vinckier F, Politis C, Mwalili S, Willems G. Tooth transplantations: a descriptive retrospective study. Int J Oral Maxillofac Surg. 2005 Oct;34(7): 745-55.
- Aslan, Unucu et al. 2010 Long-term follow-up of a patient with multiple congenitally missing teeth treated with autotransplantation and orthodontics. Angle of Orthod 80(2): 396-404
- Paulsen HU1, Andreasen JO, Schwartz O.Pulp and periodontal healing, root development and root resorption subsequent to transplantation and orthodontic rotation: a long-term study of autotransplanted premolars.Am J Orthod Dentofacial Orthop.1995 Dec;108(6):630-40.
- Escoda, G., Ed. 1999 Ciruga buccal Madrid, Editiones Ergon, S.A. Donado 2007 Cirugia, Masson
- Ahlberg, Bystedt et al.; Long term evaluation of Autotransplanted Maxillary Canines with Completed Root Formation Acta Odontologica Scandinavica 41(1): 23-31 · February 1983
- Tsukiboshi, 2001. Autotransplantation of teeth
- Akiyama Y1, Fukuda H, Hashimoto K. A clinical and radiographic study of 25 autotransplanted third molars. J Oral Rehabil. 1998 Aug;25(8):640-4.
- Czochrowska EM1, Stenvik A, Bjercke B, Zachrisson BU.Outcome of tooth transplantation: survival and success rates 17-41 years post treatment. Am J Orthod Dentofacial Orthop. 2002 Feb;121(2):110-9; quiz 193.
- Thomas, Turner et al. 1998 Autotransplantation of teeth: is there a role? Br J Orthod. 1998 Nov;25(4):275-82.
- Andreasen JO 2009 The effect of splinting upon periodontal healing after replantation of permanent incisors in monkeys Journal Acta Odontologica Scandinavica Volume 33, 1975 - Issue 6
- Northway, 2002 Autogenic dental implants American Journal of Orthodontics and Dentofacial Orthopedics 121(6):592-3 · July 2002
- Tsukiboshi, 2002 Autotransplantation of teeth: requirements for predictable success Dent Traumatol. 2002 Aug;18(4):157-80.
- Kim, Jung et al. 2005 Evaluation of the prognosis and causes of failures in 182 cases Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005 Jul;100(1):112-9.